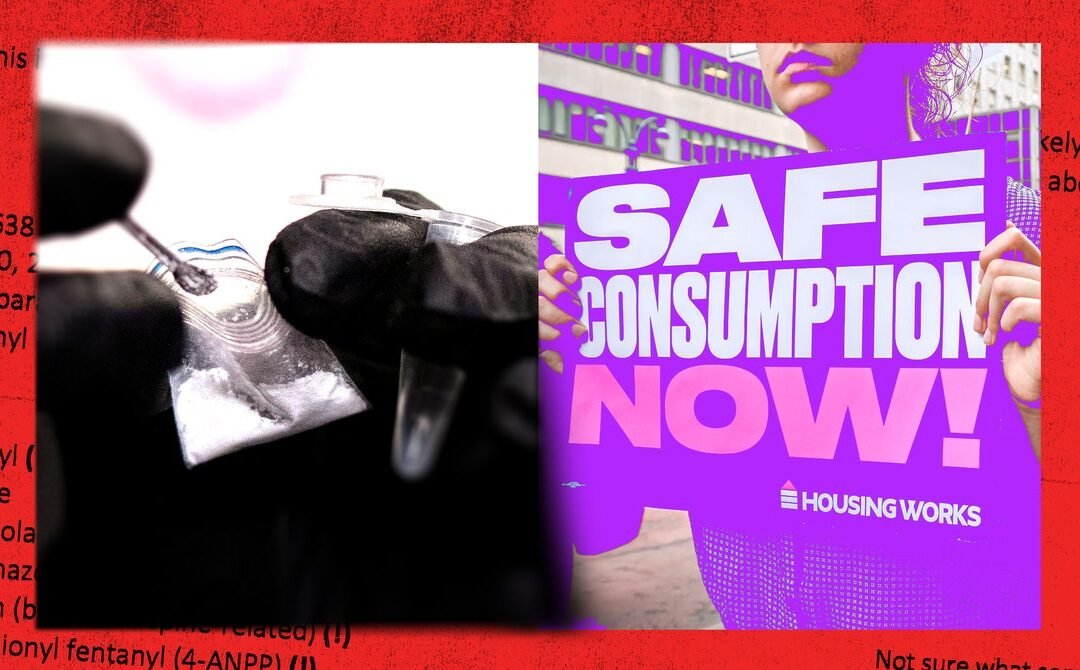
Over the past two weeks, Minnesota and Vermont took steps to explicitly legalize, fund, and expand drug-checking resources. These are major developments for drug policy. Tools like mass spectrometers and fentanyl test strips provide people with real-time information about what’s in their drugs, which can help them make more informed decisions and reduce the possibility of an overdose. What’s more, they help public health and harm reduction workers understand what is in the drug supply, a necessary prerequisite for them to respond to crises and reduce risk. More lawmakers and local organizations must follow in the footsteps of Minnesota and Vermont and implement policies that emphasize drug checking as an instrument for harm reduction, and expand its use as a community-based tool.
In addition to drug checking, we can find out what’s in the drug supply through drug supply surveillance. Most of this surveillance data is collected through law enforcement drug seizures, drug screening in clinical settings or following a death, and urine-based drug screening of people in drug treatment programs. In short, this information is often collected through punitive measures. A positive urine drug screen can result in loss of custody of a child, denial or loss of employment, and incarceration. We have baked this discrimination into law with legislation like the 1988 Drug-Free Workplace Act, which requires that employers who receive federal contracts drug test their employees. Some lawmakers have gone further, pushing to drug test people who receive government supports like food stamps and housing. And choices around who to test are often discriminatory. A study published earlier this year, for example, found that hospitals are more likely to drug test Black women who are pregnant than white women, despite no difference in rates of testing positive.
When you know what might be in the drug supply, you can be better prepared to reduce harm. You might choose to use smaller amounts, avoid mixing drugs, or not use alone. You might start carrying naloxone. But for this to be possible, we need timely and accurate communication about local drug supplies, which requires approaches that aren’t punitive or discriminatory.
Along with others at Brown University Medical School and Rhode Island Hospital, we run a pilot drug surveillance project called testRI, which takes donated samples of drugs and used paraphernalia from people across the state and tests them using a comprehensive machine at the hospital’s toxicology lab. This gives us a detailed list of all the substances that were in the sample, and allows us to understand what is in the local drug supply. Our testing data is then compiled, posted online, and distributed in the community, along with information on what substances were detected and how to reduce risk. In March, for instance, someone told us they thought they were buying fentanyl, but when we tested the sample we found xylazine, a powerful animal tranquilizer, as well. This drug can cause severe wounds and lead to prolonged sedation, which can complicate overdose responses. Once we documented the presence of xylazine, we created and distributed a zine to people in the community with information about what the drug is, how it’s showing up locally, and how people can take care of the skin wounds it causes and respond to overdoses.
We aren’t the only ones taking this kind of approach. A lab at the University of North Carolina at Chapel Hill runs a mail-based drug-checking program, where people across the country can mail in substances to be tested. And the New York City Department of Health and Mental Hygiene offers drug-checking programs at three sites, allowing people to see what’s in the substances they have on hand and giving them advice on how to reduce risk.
Pairing drug-checking programs with comprehensive drug supply surveillance efforts is critical for rapidly understanding—and responding to—changes in the supply. But for these efforts to be effective, they need to be community-driven, with the goal of reaching people where they already are. When we worked with local partners to post on Instagram and Twitter and distribute zines and other printed materials, it led to funding for wound care kits that are distributed by harm reduction agencies in the state, and additions to the state’s overdose dashboard.